A new study led by Dr. Marc Martí-Renom (CNAG), Dr. Eduard Batlle and Dr. Carme Cortina (IRB Barcelona), in collaboration with Revolution Medicines, shows that metastatic colorectal cancers (mCRC) are highly diverse, made up of tumor cells that adopt different states and display distinct properties. Within a given tumor, cells can rapidly shift from one state to another — a key cancer feature known as transcriptional plasticity. This flexibility enables KRAS-mutant mCRC to withstand treatment with a novel targeted compound that selectively inhibit oncogenic KRAS signaling.
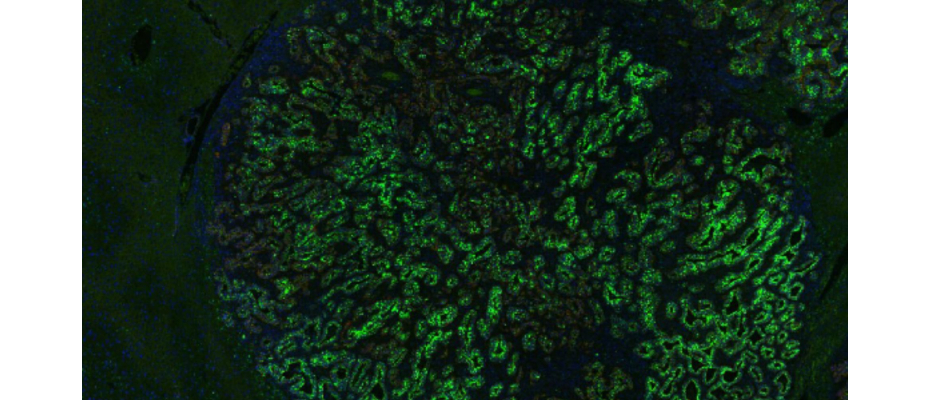
Using preclinical models of mCRC, the authors show that oncogenic KRAS induces a cell state associated with metastasis and poor prognosis. However, when mutant KRAS activity is blocked with a KRAS mutant-selective inhibitor, tumor cells switch from this state to a stem-like state marked by LGR5. These LGR5⁺ cells depend less on KRAS signaling, which may explain the limited benefit of KRAS-targeted approaches in colorectal cancer.
To characterise these dynamic transitions, the Structural Genomics Group at CNAG, with Meritxell Novillo as second author, led the RNA sequencing and applied advanced epigenetic techniques such as Hi-C, ATAC-seq and ChIP-seq. These approaches enabled the team to uncover how changes in gene regulation, rather than new DNA mutations, drive the switch in cell identity and support tumour plasticity as a key mechanism of therapeutic resistance.
The team finds that this switch is driven by changes in gene-reading programs that control which genes ar
e turned on or off and define cell identity, rather than by new DNA mutations—highlighting plasticity as the main escape route.
In preclinical models of colorectal cancer metastasis, combining KRAS-pathway inhibition with strategies that eliminate the emergent LGR5⁺ population produced stronger, longer-lasting responses.
Take-home message: In KRAS-mutant CRC, treatment pressure can redirect cell states rather than simply kill them. Tackling heterogeneity and plasticity—especially the emergence of the LGR5⁺ state—may be essential to improve outcomes.
The study also involved researchers from VHIO (Barcelona), the Research Institute of Molecular Pathology, (IMP, Vienna), CIBERONC, Imperial College (London), the Francis Crick Institute (London), CSIC’s Instituto de Investigaciones Biomédicas Sols-Morreale (Madrid) and IdiPAZ (Madrid).
REFERENCE ARTICLE
Centonze, Alessia, et al. ‘A Plastic EMP1+ to LGR5+ Cell State Conversion as a Bypass to KRAS-G12D Pharmacological Inhibition in Metastatic Colorectal Cancer’. Cancer Discovery, Oct. 2025. DOI.org (Crossref),
https://doi.org/10.1158/2159-8290.CD-25-0679.